Last week an article written by Prof. Catherine Brooks was published by Scientific American. In it, Brooks asserted that people don’t trust scientists and questioned whether science communicators are the problem by “relying too much on gripping headlines or in trying to get science information to viral” which might be “somehow undermining the critical role of trust in scientifically based work”.
Now, I’m a bench scientist. But I’m also an amateur science communicator. I blog and tweet, I write occasional news articles, I’ve podcasted fortnightly for over three years, I’ve been actively involved in skepticism for over six years. I give talks – to lay audiences across the world, to academics and to industry collaborators. I do workshops with kids of all ages.

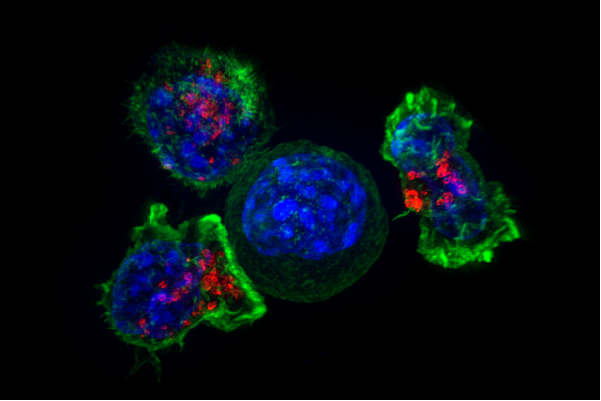
I talk about science with every person I meet – from taxi drivers to GPs, from family to friends, I once did a science test in the changing rooms of a rugby club with a rugby kicker. My mother-in-law left school at 16 and hadn’t thought about science for decades but she still asks me how my cells are doing. We talk about the science behind her vision problem and how cancer works.
I work in academia – but I live in science communication.
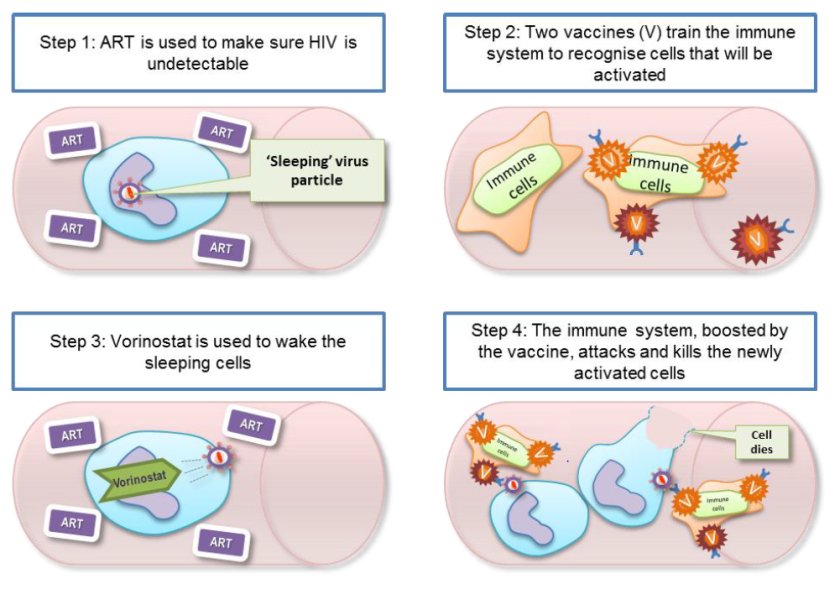
I understand the frustration that some people are losing their trust in science. I find it hard to see so many people, especially people living with cancer, turn to conspiracy theories. But I also see, every day, a lot of people who trust science.

The problem is not with making science popular using YouTube or Instagram. The problem lies precisely with the solution Brooks suggests. In her article Brooks says “we need to keep science information findable in a busy digital culture by simply presenting the data while relying on emotional appeals to a lesser extent”. But findable isn’t the same as seen. And seen isn’t the same as engagement.
People know that they can find science information “out there”. Sticking with my Mother-in-law, her favourite response to any question is “Google it”. Anything is findable. But do people know that they can understand that science without speaking the academic language? Or do they know it can be fun, exciting or awe-inspiring? Instead of those drab school lessons they had decades ago which left them putting science in a box labelled “not for me”.

Science communication is far more than just communicating science. It’s about knowing your audience, knowing what engages them and the ideas they relate to. And sometimes that means finding a way to appeal to their emotions. That shouldn’t be at the expense of good science, but what’s the point in doing good science if you can’t convey the benefit of it? Sometimes, science communication is about persuading your audience to open up that box, and challenge the idea that science isn’t for them. It’s about making science accessible for everyone.

Every fortnight for Skeptics with a K, I read through many, many articles that report science dreadfully – either they miss the point of the study, or they misrepresent it, or they leave out the science of a topic entirely. But for all its faults, there are many things we can learn from the media, too. Sure, clickbait and listicles drive us all spare…but the media uses them because they work. We can learn something about human nature from which types of article the media prefers. Sure an article headlined “top ten things….and you won’t believe number nine!” might be frustrating, but why can’t we write a list that our audiences will engage with? Like that wonderful article from Cancer Research UK: Don’t believe the hype – 10 persistent cancer myths debunked (which I still re-read every few months despite it being written nearly five years ago). And maybe we’re all frustrated by those YouTube videos your great aunt Irma posts on Facebook about “the one cancer cure your doctors won’t tell you about” but maybe we can use that video model to teach people critical thinking.
Remove the emotion from science and you leave scientists sat in their ivory tower as elite academics who don’t know how the real world works. But out here in the real world – a lot of science communicators are using the best techniques to engage with people from all walks of life and bring science in to the hands of the “people” – where it belongs.