Recently, Professor Chris Exley from Keele University claimed that his research “provides the strongest indication yet that aluminium is a cause of ASD”. In an article originally published in the Hippocratic Post and reproduced by the Daily Mail, Exley claimed that brain tissue from five donors diagnosed with Autism Spectrum Disorder (ASD) contained “some of the highest values yet measured in human brain tissue” of aluminium. He postulated “perhaps we now have the link between vaccination and autism”.
This controversial claim comes almost two decades after Andrew Wakefield published the now discredited and retracted research into ASD and the measles, mumps and rubella (MMR) vaccine which was linked to a decline in vaccination rates and recent outbreaks of measles.
I spoke to Tom Chivers from Buzzfeed about my concerns with this paper. In his article you can read concerns from myself and eminent academics Professor Dorothy Bishop and Professor Jonathan Green, renowned experts in neurodevelopmental biology and child and adolescent psychiatry respectively.
Such a controversial claim which can affect the health of children worldwide really needs some solid supporting evidence. So, let’s take a look at the paper itself.
Aluminium in brain tissue in autism
The paper is due to be published in the Elsevier Journal of Trace Elements in Medicine and Biology in March 2018 and the accepted paper is available to read online. The authors introduce the study saying “we have measured aluminium in brain tissue in autism and identified the location of aluminium in these tissues”. The paper can be split into two sections.
Section one
The authors measured the levels of aluminium in brain tissue taken from five donors aged 15 to 50 who had all been diagnosed with ASD prior to their deaths. They took 0.3g tissue samples for four (occipital, frontal, temporal and parietal lobes) or five (they added hippocampal tissue where it was available) brain regions. They measured three replicates of each brain region using spectrometry.
The problems with the methods and data from this section are three-fold:
- The authors took samples from only five brains – all five donors had died with a diagnosis of ASD. There were no healthy control samples used anywhere in this study. This is a particular problem because without a healthy control, it is impossible to really say whether the aluminium levels measured in the brains of the donors is actually higher than that of a non-autistic brain. There is nothing to compare the measurements to.
- Importantly, the authors do not provide information on how the donors died. We have to take their word that the cause of death does not account for variation in brain levels of aluminium. An important part of the scientific publication framework is that this sort of information should be easily available to the reader. We need to be able to come to our own conclusions based on the data presented. That this information is missing is quite concerning.
- Finally, in some cases the three replicates from each brain region per donor did not corroborate each other. In one case there were three measurements of 0.01, 0.64, and 18.57μg/g. Similarly, another donor had measurements of 2.44, 1.66, and 22.11 and another, 1.71, 1.64, and 17.10μg/g. The authors averaged these data, however such an average does not represent any of the three measurements and is an inappropriate way to analyse these figures. In fact, such variation between measurements might even hint at an anomalous result, which requires further assessment to adequately rule out.
Section two
In the second section of this paper the authors took samples of brain tissue from the valuable Oxford Brain Bank. Again, they took tissue from a selection of donors who had been diagnosed with ASD before their death. Again, the authors failed to express how the donors died. The authors took samples from 10 donors aged 14 to 50 and stained them with a dye that specifically sticks to aluminium. The dye can then be visualised with a fluorescent microscope to see where in the brain tissue it can be seen.
Again, the issues with this section are three-fold
- This section also lacks the use of ‘healthy’ controls. The authors do show presence of aluminium in the tissue samples of their ASD donors but we have no indication of whether this is, in fact, more than we might see in a healthy brain.
- This section is also lacking a positive control – a sample that has a known amount of aluminium in it. This is important for interpreting the staining of the dye; if the dye is very sensitive then we might see loads of staining for just a small amount of aluminium. We need to compare it to a known sample.
- Later in their interpretation of these data the authors discuss the presence of aluminium in specific cell-types which they surmise might be lymphocytes. However, they do not use any detectable markers to propose this, they base it only on how the cells look. Cell appearance (also known as morphology) is a useful initial indicator of cell-type but it is important to confirm this using specific markers for those cells.

Overall the data from this paper is insufficient to draw the conclusions made in the Hippocratic Post and The Daily Mail and it is my concern that such reporting is irresponsible. While the two articles conclude that aluminium present in the brains of people with ASD might be caused by vaccination, there is no investigation whatever into the source of such aluminium in this study. There are no data presented in this paper sufficient to implicate vaccination in these findings. To draw the link between aluminium in the brain of people with ASD and vaccinations makes for a striking headline but the data do not support this claim and it could therefore be viewed as scare-mongering.
I am surprised that this paper was published in the Journal of Trace Elements in Medicine and Biology because the lack of control data makes the findings inconclusive. I am yet more surprised that this inconclusive data has been reported in such a paper as The Daily Mail, when such media attention can lead to parents making potentially dangerous decisions for the health of their children.
Please let me know below what you think about the reporting of this science?







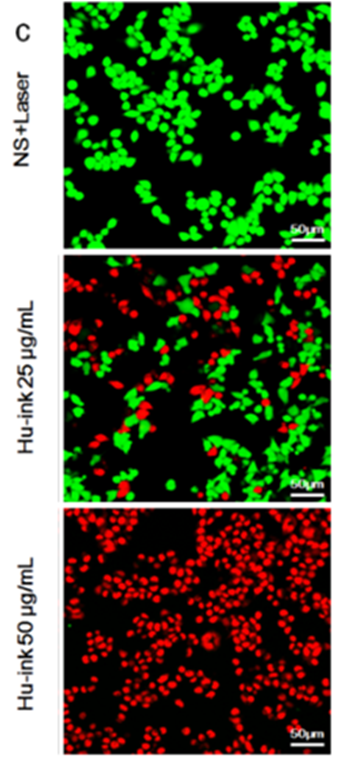
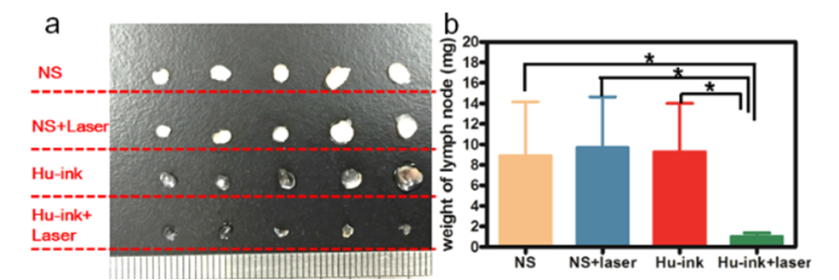




 Image: figure from the
Image: figure from the 

